In our office, we frequently get patients requiring root canal treatment caused by tooth decay. Surprisingly, many patients are unaware of what tooth decay is therefore many think that it's not there. The questions we get asked quite frequently is: what is tooth decay and what causes it? What can be done to prevent it?
What is tooth decay?
Tooth decay is damage that occurs when bacteria in our mouths create acids that begin to eat away at our teeth. This action leads to a hole in a tooth, also called a cavity. If not treated, tooth decay can cause pain, infection and possibly tooth loss.
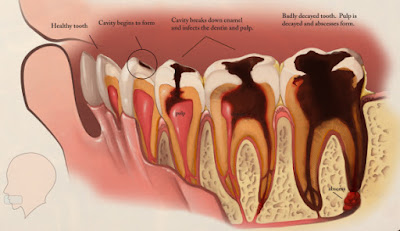
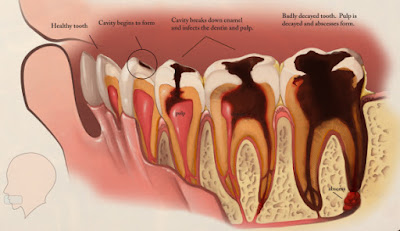
Our teeth have three layers: the enamel, the dentin and the pulp chamber. The enamel is the hard outer layer that is visible to the eye. The dentin is the middle layer and the third layer is the pulp chamber, this is where the nerves and blood vessels are located. The deeper the decay goes the more damage there is.
What causes tooth decay?
The culprits: bacteria and food. Have you ever notice a sticky, sort of clear substance on your teeth? Well, that substance is called plaque and it's always forming on our teeth. Plaque contains bacteria which feeds on the sugars of the food that we eat. This causes acids to develop that attack our teeth after we eat. Over time, these acids destroy the outer layer of the tooth leading to tooth decay.
What can one do to prevent tooth decay?
Brush and floss your teeth regularly. Attempt to visit your dentist on a regular bases for checkups and cleanings. Avoid eating foods that are high in sugar. Use fluoride based tooth products. Fluoride helps by making teeth more resistant to acids. Fun fact: fluoride is added to many public water supplies. Saliva helps wash away food and sugars so try to keep yourself hydrated. Avoid smoking.
 A dentist will do treatment according depending on the severity of the tooth decay. In the early stages of tooth decay, you might be able to stop it by brushing with fluoride toothpaste or fluoride treatment. If decay has already eaten through the outer layer of the tooth you might need more dental treatment. If the tooth hasn't gone through the middle layer and it's created a cavity, a dentist will do a filling after the decay is removed. If the decay is severe and the tooth is badly damaged, a crown or cap is made as a replacement for the tooth. If the decay has eaten through to the third layer, then a root canal treatment is needed. This removes the diseased pulp from the tooth. If the tooth is severely damaged, to a point where no treatment can be done to save it, an extraction is done.
A dentist will do treatment according depending on the severity of the tooth decay. In the early stages of tooth decay, you might be able to stop it by brushing with fluoride toothpaste or fluoride treatment. If decay has already eaten through the outer layer of the tooth you might need more dental treatment. If the tooth hasn't gone through the middle layer and it's created a cavity, a dentist will do a filling after the decay is removed. If the decay is severe and the tooth is badly damaged, a crown or cap is made as a replacement for the tooth. If the decay has eaten through to the third layer, then a root canal treatment is needed. This removes the diseased pulp from the tooth. If the tooth is severely damaged, to a point where no treatment can be done to save it, an extraction is done.
If you believe you might have tooth decay, please visit your dentist for a more accurate diagnosis.
What is tooth decay?
Tooth decay is damage that occurs when bacteria in our mouths create acids that begin to eat away at our teeth. This action leads to a hole in a tooth, also called a cavity. If not treated, tooth decay can cause pain, infection and possibly tooth loss.
Our teeth have three layers: the enamel, the dentin and the pulp chamber. The enamel is the hard outer layer that is visible to the eye. The dentin is the middle layer and the third layer is the pulp chamber, this is where the nerves and blood vessels are located. The deeper the decay goes the more damage there is.
What causes tooth decay?
The culprits: bacteria and food. Have you ever notice a sticky, sort of clear substance on your teeth? Well, that substance is called plaque and it's always forming on our teeth. Plaque contains bacteria which feeds on the sugars of the food that we eat. This causes acids to develop that attack our teeth after we eat. Over time, these acids destroy the outer layer of the tooth leading to tooth decay.
What can one do to prevent tooth decay?
Brush and floss your teeth regularly. Attempt to visit your dentist on a regular bases for checkups and cleanings. Avoid eating foods that are high in sugar. Use fluoride based tooth products. Fluoride helps by making teeth more resistant to acids. Fun fact: fluoride is added to many public water supplies. Saliva helps wash away food and sugars so try to keep yourself hydrated. Avoid smoking.
How does one know they might have tooth decay?
The most common symptom is a toothache. Though tooth decay usually doesn't cause symptoms until you have a cavity or infected tooth. Another sign is swelling in the gums near the sore tooth. This could be a sign of severe tooth decay or an abscessed tooth. You may experience bad breath or a bad taste in your mouth. You might also experience spots on your teeth usually colored white, gray, brown or black.
Once you experience a toothache, please see a dentist. The pain might go away for a bit but the tooth decay will just keep growing. Without treatment, the decay will get worse and you might lose a tooth.
Once you get diagnosed with tooth decay, how is it treated?
 A dentist will do treatment according depending on the severity of the tooth decay. In the early stages of tooth decay, you might be able to stop it by brushing with fluoride toothpaste or fluoride treatment. If decay has already eaten through the outer layer of the tooth you might need more dental treatment. If the tooth hasn't gone through the middle layer and it's created a cavity, a dentist will do a filling after the decay is removed. If the decay is severe and the tooth is badly damaged, a crown or cap is made as a replacement for the tooth. If the decay has eaten through to the third layer, then a root canal treatment is needed. This removes the diseased pulp from the tooth. If the tooth is severely damaged, to a point where no treatment can be done to save it, an extraction is done.
A dentist will do treatment according depending on the severity of the tooth decay. In the early stages of tooth decay, you might be able to stop it by brushing with fluoride toothpaste or fluoride treatment. If decay has already eaten through the outer layer of the tooth you might need more dental treatment. If the tooth hasn't gone through the middle layer and it's created a cavity, a dentist will do a filling after the decay is removed. If the decay is severe and the tooth is badly damaged, a crown or cap is made as a replacement for the tooth. If the decay has eaten through to the third layer, then a root canal treatment is needed. This removes the diseased pulp from the tooth. If the tooth is severely damaged, to a point where no treatment can be done to save it, an extraction is done.If you believe you might have tooth decay, please visit your dentist for a more accurate diagnosis.

Comments
Post a Comment